What will the landscape of general practice look like a decade from now?
FUNDING ISSUES
Presently, as reported in the Pulse article, NHS spending on primary care falls short of what’s necessary to sustain it. Despite calls for increased funding from the government, proposed solutions often miss the mark, failing to address the unique challenges faced in primary care.

One glaring issue is the retention of GPs, who should be leading the charge in primary care. Many cite burnout, financial constraints, and administrative hurdles as obstacles hindering their ability to provide essential services.
Recognising the need for flexibility to combat burnout, there’s a push for GPs to have more varied roles. Yet, financial, logistical, and bureaucratic barriers persist, discouraging locum and salaried GPs from seeking partnerships, which is still the most viable way forward for primary care. This points to a fundamental misunderstanding of the essence of primary care, with potential repercussions for its future.
VALUE PROPOSITION
A fundamental question arises: How does primary care impact both individual health and population well-being? While evidence suggests its value to the broader population is well appreciated, it’s often undervalued in disease-specific care. Despite its holistic approach, primary care remains under-appreciated, fostering a preference for fragmented care that overlooks the interconnected medical, social, and environmental factors influencing health.
Support for primary care must reflect our value for and understanding of how it functions. Should primary care receive winter pressure uplift, when disease presentations go above a certain frequency? It comes down to value.
A unified desire for a successful primary care system exists among providers, recipients, and funders. However, achieving this vision requires alignment, which is currently lacking. GPs seek time to provide quality care, while funders emphasise efficiency in disease specific management and patient volume, leaving recipients caught in the middle.
What strategies can enhance the success of GP practices within the current framework? Successful practices have broadened their scope beyond basic services, by offering specialised clinics and procedures. Evidence suggests that these disease specific management are more valuable to the payers of care. Hence, the proliferation of specialised clinics like frailty clinics, functional illness, dermatology, diabetes, menopause etc. Facilitating early adoption of these portfolio roles by salaried and locum GPs, where possible, should be highly encouraged and supported. It’s been recognised that having a portfolio career enhances staff retention.
Another suggestion would be addressing funding challenges in primary care. This requires innovative approaches. One avenue involves recognising the GPs’ role in disease management and advocating for policy changes to incentivise the broad primary care consultations. Standardising consultation systems, such as incorporating the International Classification of Primary Care (ICPC) framework, can reward early disease interventions and administrative interactions, improving care continuity and coordination.
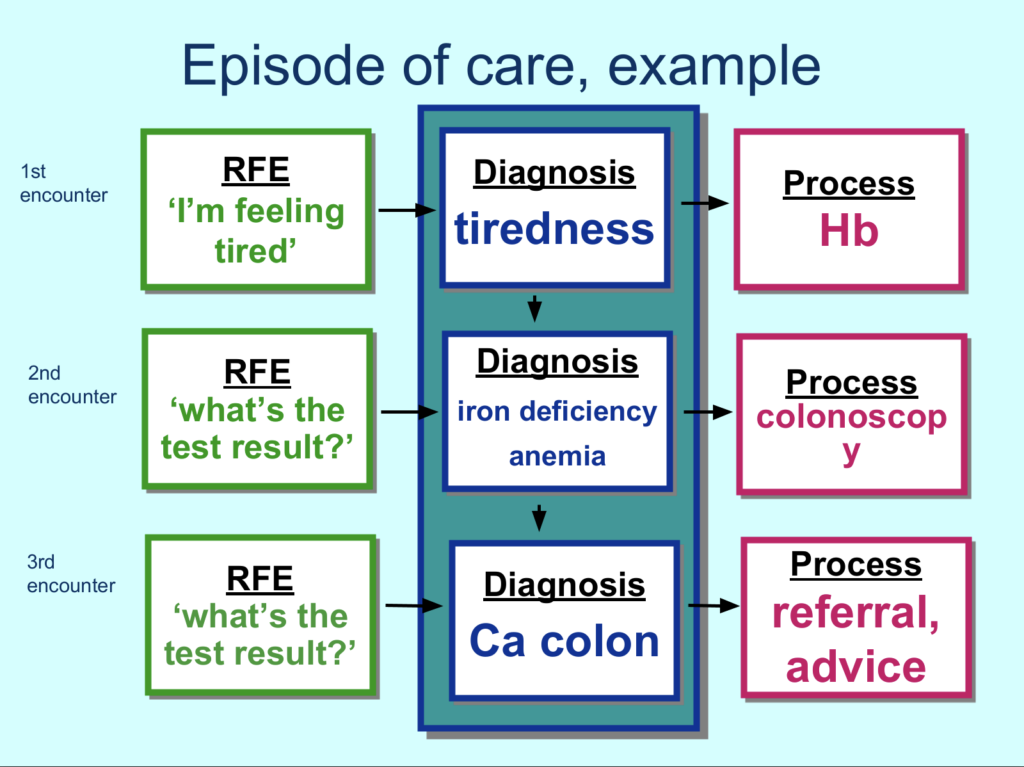
Furthermore, leveraging data from the ICPC framework will provide insight into condition management and associated costs, facilitating informed decision-making and improved resource allocation. This approach could enhance funding mechanisms, in addition to the current QOF indicators, enabling primary care providers to deliver impactful services that all parties can value. Proficiency in appointment management is also crucial for optimising workforce capacity, though often overlooked and unrewarded.
TRAINING NEEDS – EDUCATION FOR WHAT PURPOSE?

Additionally, reforming GP training programmes is vital to align with the evolving vision of primary care. Restructuring the curriculum to prioritise extended placements in general practice equips trainees with the skills and perspective needed for partnership roles. By instilling a sense of purpose and pride in primary care, this approach can reshape perceptions among aspiring GPs, fostering a workforce committed to these broad but unique high value primary care activities.
Overall, envisioning the future of general practice requires collaborative efforts to innovate the current funding categories, facilitate role adjustments for disease management based on local needs, and create contemporary VTS training schemes that draws its curriculum from the partnership model mindset. By showcasing the value of the broad primary care consultations in terms that all interested parties can relate to, we can hope to see, a decade from now, the primary care system that meets the needs of both providers, payers and recipients, ensuring a healthier future for all. Share your thoughts on this vision in the comments below.
Read our article on 3 Strategies for a Stronger Primary Care Workforce.



