What will the landscape of general practice look like a decade from now? This question has never been more urgent. As we approach 2026, NHS organisations face efficiency targets ranging from 1.6% to 11%, with more than half predicting they will not meet their targets. Meanwhile, the GP partner workforce has lost 470 full-time equivalent partners in just the last year, continuing a decade-long decline of 6,397 FTE partners since 2015.
To answer this critical question, we must confront three interconnected crises: a funding shortfall that threatens the viability of primary care, a fundamental misalignment in how we value and measure primary care’s contribution, and a partnership model in free fall. Yet amidst these challenges lies an unprecedented opportunity for transformation through the government’s 10 Year Health Plan and the shift toward neighbourhood-based care.
The Funding Crisis: Beyond the Headlines

The Real Numbers Behind the Crisis
The NHS needs an immediate cash injection of around £8.5 billion per year over the next four years to make up a £32 billion shortfall in funding. For primary care specifically, the Darzi report found that funding for primary care had fallen by a quarter since its peak in 2024, creating a challenging environment where activity has increased as funding has declined.
The 2025/26 GP contract offers a glimmer of hope with a 7.2% total increase to core funds, the largest increase in investment in over a decade. However, this is immediately eroded by increases to minimum wage and employers’ National Insurance contributions, with NHS England estimating the real-terms increase at only 4.8%.
The Partnership Crisis: A System Under Siege
The numbers paint a stark picture. GP partner numbers have dropped by around 25% over the past decade in England, while the number of salaried GPs has risen by 86%, now representing 49% of the workforce. More alarmingly, between June 2024 and September 2025, the number of full-time equivalent partners declined by 4.1%, and the number of partners under age 40 declined by 17%.
The age profile tells an ominous story. In September 2025, only 10.5% of the partner workforce was aged under 40, roughly half the proportion from September 2015, while the proportion aged over 60 rose from 9.4% to 15.5%. We are approaching a cliff edge where partners retire with insufficient qualified GPs to replace them.
Are Partnerships Struggling?
According to the 2024 GP trainee survey, responsibility for practice workload remains the top deterrent for trainees considering partnership, growing from 56% in 2019 to 64% in 2024, while financial commitment is cited by 60% of trainees. Even more concerning, administrative workload emerged as a growing concern, cited by 75% of trainees in 2024 compared with 49% in 2019.
The British Medical Association reports a marked increase in the proportion of practice income being consumed by expenses, leaving less available for partner drawings. This creates a vicious cycle: rising costs squeeze partner income, making partnerships less attractive, which leads to fewer partners, which increases workload and financial pressure on remaining partners.
The Value Proposition Crisis: What Is Primary Care Worth?
The Fundamental Question
How does primary care impact both individual health and population well-being? This question lies at the heart of the funding crisis. While evidence suggests primary care’s value to the broader population is appreciated, it remains systematically undervalued in disease-specific care models that dominate NHS funding mechanisms.
Primary care’s holistic approach—addressing the interconnected medical, social, and environmental factors influencing health—is precisely what makes it invaluable yet difficult to quantify using traditional metrics. This creates a destructive paradox: the very qualities that make primary care effective are those that current funding models fail to reward.
The Alignment Problem: A Three-Way Disconnect
We face a fundamental misalignment between three key stakeholders:
GPs seek: Time to provide quality, holistic care that addresses patients’ complex, interconnected health needs. They want to practice the comprehensive medicine they were trained to deliver, building long-term relationships that improve outcomes.
Funders emphasize: Efficiency in disease-specific management, patient volume, and measurable quality outcomes tied to specific conditions. They seek value through traditional healthcare metrics focused on individual disease management.
Recipients need: Accessible, coordinated care that addresses their health in context of their lives, with continuity of relationship and seamless navigation of complex health systems.
This three-way tension creates a system where everyone loses. GPs experience burnout trying to meet incompatible demands. Funders see rising costs without proportional outcomes. Patients face fragmented care that treats diseases rather than people.
The Neighbourhood Health Revolution: Opportunity Amidst Crisis
The 10 Year Health Plan: A Paradigm Shift
The government’s 10 Year Health Plan commits that the share of expenditure on hospital care will fall over the next three to four years with proportionally greater investment in out-of-hospital care, including neighbourhood health centres. This represents the most significant structural shift since the NHS’s founding.
Neighbourhood health centres will house services under one roof, eventually open 12 hours a day, six days a week, bringing historically hospital-based services into the community, including diagnostics, post-operative care and rehabilitation. These centres will also offer integrated support services like debt advice, employment support, and lifestyle interventions—recognizing that health is determined by far more than medical care alone.
Evidence from Early Adopters
The model isn’t theoretical. Where neighbourhood health teams have been trialled in England, they have significantly reduced hospital use—in Derby, integrated teams led to 2,300 fewer category 3 ambulance callouts and 1,400 fewer short hospital stays among the over-65 population within a year.
From September 2025, the government began working with 42 selected sites to accelerate neighbourhood health services, prioritised in areas where healthy life expectancy is lowest. These pioneers will test what works and provide a roadmap for national rollout.
However, significant challenges persist. The plan does not refer to traditional GP practices, begging the question: will GP practices be replaced by or become integrated with new neighbourhood health centres? This uncertainty creates anxiety among GP partners who have invested their careers and finances in existing practices.
The government has indicated an intention to draw on private sector funding through public-private partnerships, with a final decision expected by the 2025 autumn budget. The implications for GP autonomy and the partnership model remain unclear.
Strategic Solutions for an Optimistic Radical Future
1. Expanding the Value Proposition Through Portfolio Roles
Successful practices have already adapted by broadening their scope beyond basic services. The proliferation of specialised clinics—frailty, functional illness, dermatology, diabetes, menopause—reflects both clinical need and economic reality. Evidence suggests disease-specific management and research are more valued by healthcare payers, creating a pragmatic pathway for practices to secure sustainable income.
For Primary Care Networks, the Additional Roles Reimbursement Scheme has been expanded for 2025/26, with caps on recruitment removed, giving PCNs full autonomy over their patient-facing workforce. This flexibility enables practices to build multidisciplinary teams tailored to local needs.
The key is facilitating early adoption of portfolio roles by salaried and locum GPs. Research demonstrates that portfolio careers enhance staff retention by providing variety, preventing burnout, and offering professional development. This addresses both the partnership crisis and workforce sustainability.
2. Transforming Funding Through Data-Driven Classification
The current funding model fundamentally fails to capture primary care’s value. Quality and Outcomes Framework (QOF) indicators measure disease-specific outcomes but miss the broader impact of early intervention, continuity of care, and holistic management.
The ICPC Framework Could Be A Game-Changing Solution
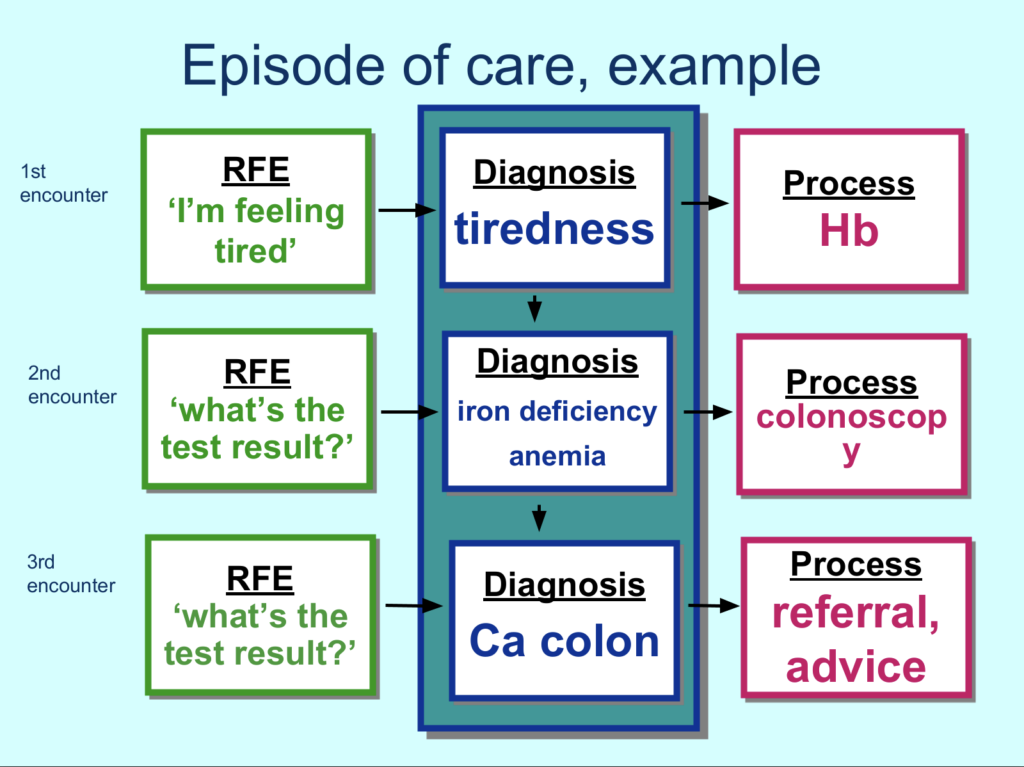
The International Classification of Primary Care (ICPC-2) offers an insightful approach. ICPC-2 classifies patient data and clinical activity in primary care domains, allowing classification of the patient’s reason for encounter, problems managed, interventions, and ordering of these data in an episode of care structure.
Unlike the International Classification of Diseases (ICD), which was designed for mortality and hospital statistics, ICPC contains codes mainly based on frequencies encountered in primary care with a level of detail appropriate for primary care.
Practical Implementation
Standardising consultation systems around ICPC-2 framework would:
Reward early intervention: Capture the value of GPs identifying and managing conditions before they require specialist care, reducing downstream costs and improving outcomes.
Recognise administrative work: Code the substantial time GPs spend on care coordination, documentation, and system navigation—currently invisible and unrewarded.
Improve care continuity: Track episodes of care across multiple consultations, demonstrating the value of longitudinal relationships.
Enable data-driven resource allocation: ICPC-2 supports quality improvement initiatives by enabling tracking of health outcomes and effectiveness of interventions over time, allowing healthcare providers to identify patterns and implement evidence-based strategies.
By integrating ICPC-2 with existing QOF indicators, we create a comprehensive funding model that values both disease-specific outcomes and the broader contributions of primary care. This data would demonstrate to funders, policymakers, and the public exactly what primary care delivers and what it costs to deliver it well.
3. Revolutionising Appointment Management
Proficiency in appointment management is crucial yet often overlooked and unrewarded. The 2025/26 contract updates the capacity and access payment, with expansion of online consultation tools to allow patients to submit requests at any time during core hours.
Effective appointment management isn’t just about availability—it’s about matching the right patient with the right clinician at the right time. Advanced demand and capacity modeling, intelligent triage systems, and flexible workforce deployment can dramatically improve efficiency without increasing staff numbers.
This requires investment in training, technology, and analytical capability. Practices that excel at appointment management optimise workforce capacity, reduce waste, improve patient satisfaction, and create better working conditions for clinicians. Yet current funding models don’t recognise or incentivise this expertise.
4. Training for Tomorrow: Aligning Education with Reality
The Current-State Training Crisis
Despite commitments to increase GP numbers, including a pledge of 6,000 more GPs by 2024, the number of fully qualified full-time equivalent GPs in England has been consistently falling. This isn’t just a recruitment problem—it’s a retention crisis beginning at training.
The fundamental issue: are we training GPs for a partnership model that’s collapsing while also failing to prepare them for the neighbourhood-based, integrated care model that’s emerging? This disconnect leaves newly qualified GPs confused about their career path and uncertain about entering partnership.

Restructuring GP Training for the Future
Reforming GP training programs must align with the evolving vision of primary care:
1. Extended Primary Care Placements
Restructure the curriculum to prioritise extended placements in diverse general practice settings. Trainees need exposure to multiple models to understand the full spectrum of primary care delivery.
2. Partnership Model Education
Despite its challenges, the partnership model remains central to primary care’s flexibility and innovation. Training must include practical education on practice management, financial literacy, leadership, and the business aspects of running a practice. The current curriculum treats these as peripheral when they’re actually foundational.
3. Integrated Care Competencies
Trainees must develop skills in multidisciplinary team working, care coordination, population health management, and data analytics. NHS England guidance identifies six core components of neighbourhood health services, requiring integrated health and care services and workforce at the most local level within neighbourhoods. Tomorrow’s GPs must lead these integrated teams.
4. Portfolio Career Development
Build portfolio career thinking into training from the outset. Expose trainees to specialized clinics, leadership roles, quality improvement projects, and research opportunities. Help them see general practice as a platform for diverse, fulfilling careers rather than a single, narrowly defined role.
5. Instilling Purpose and Pride
Most importantly, training must reshape perceptions of primary care. Rather than portraying general practice as the fallback option for those who don’t pursue hospital specialties, we must celebrate it as the most challenging, rewarding, and impactful medical career—which it genuinely is.
By showcasing primary care’s unique value in terms meaningful to aspiring doctors, we can foster a workforce committed to the broad, high-value activities that define excellent primary care. This means highlighting impact on population health, continuity of relationships, diagnostic complexity, and the privilege of caring for patients across their entire life course.
A Radical And Integrated Vision for 2035
Envisioning the future of general practice requires acknowledging uncomfortable truths while embracing transformative opportunities. The current trajectory is unsustainable—but change is possible with courage and collaboration.
Achieve value-based primary care: Establish funding models that fully reflect primary care’s contributions to individual health, population wellbeing, and system efficiency. Move beyond disease-specific metrics to holistic measures of health and quality of life.
Mature neighbourhood health systems: Create seamless integration between primary, community, social, and specialist care. Patients experience coordinated journeys through health systems rather than fragmented episodes.
Sustainable workforce: Build a GP workforce where partnership is attractive and viable, portfolio careers are standard, and retention rates improve because doctors have satisfying, manageable workloads with appropriate compensation.
Evidence-based iteration: Use comprehensive data from Episode of Care templates and other sources to continuously refine what works, abandon what doesn’t, and adapt to emerging needs and technologies.
A Call to Action
The decade ahead will determine whether primary care thrives or merely survives. Success requires collaborative effort from everyone with a stake in the future of healthcare:
For policymakers: Move beyond rhetoric to concrete funding reform. Recognize that investing in primary care isn’t cost—it’s the most effective healthcare investment possible. Support the transition to neighbourhood health while preserving what works in current models.
For commissioners and ICBs: Embrace innovative funding approaches. Pilot ICPC-2 implementation. Create incentives that align with primary care’s actual value rather than artificially narrowed metrics.
For practice leaders: Don’t wait for perfect solutions. Innovate within current constraints through specialized clinics, portfolio working, and partnership with PCNs. Collaborate and share business successes and failures to accelerate collective learning.
For educators: Revolutionise GP training now. The doctors graduating today will shape primary care in 2035. Equip them with skills for integrated, neighbourhood-based care while instilling pride in primary care’s unique contribution.
For GPs, especially early career GPs: Engage with these changes rather than retreating from them. Your voice matters in shaping the future. Consider partnership, develop portfolio careers, lead quality improvement, and advocate for the value of what you do every day.
Conclusion: Transforming Crisis into Opportunity
The landscape of general practice in 2035 will look dramatically different from today—but whether that difference represents transformation or collapse depends on choices we make now. The convergence of funding crisis, workforce exodus, and systemic reform creates unprecedented pressure. Yet within this pressure lies the catalyst for long-overdue change.
By showcasing primary care’s value in terms all stakeholders understand, by reforming funding to reward what matters, by training doctors for tomorrow’s reality rather than yesterday’s model, and by building integrated neighbourhood health systems that place primary care at their heart, we can create a healthcare system that truly serves population health.
The vision is ambitious but achievable. The alternative—continuing on our current trajectory—is simply unacceptable. Primary care is too important to fail, too valuable to undervalue, and too fundamental to health and wellbeing to allow it to wither from neglect.
A decade from now, we can look back on 2025 as the moment when primary care began its transformation from the neglected foundation of the NHS to the celebrated cornerstone of a health system that keeps people healthy, provides care where they need it, and makes efficient use of every resource. That future is within reach—if we have the courage to build it.
What’s your vision for the future of general practice? How will you contribute to making it reality?
Read our article on 3 Strategies for a Stronger Primary Care Workforce.
References:
STANGE, K.C., MILLER, W.L. and ETZ, R.S. (2023). The Role of Primary Care in Improving Population Health. The Milbank Quarterly, 101(S1), pp.795–840. doi:https://doi.org/10.1111/1468-0009.12638.
Parr, E. (2024). Inflation ‘forced’ NHS England to Cut Primary Care Funding Last Year. [online] Pulse Today. Available at: https://pulsetoday.co.uk/news/practice-personal-finance/inflation-forced-nhs-england-to-cut-primary-care-funding-last-year/ [Accessed 10 Dec. 2025].



