Introduction
The healthcare sector stands at a critical juncture. As we navigate unprecedented workforce pressures, the question is no longer whether we should prioritise staff wellbeing, but rather how we can strategically embed it within our organisational DNA. This reflective piece explores the evolution of wellbeing strategy within the NHS context, examining how a new measurement framework, person-centred approaches, and team dynamics converge to create sustainable, high-performing healthcare organisations.
Reflection on Current Practice in Workforce Wellbeing
The Paradigm Shift: From Reactive to Proactive
My exploration of contemporary wellbeing frameworks reveals a fundamental shift in how healthcare organisations conceptualise workforce health. The revised NHS Health and Wellbeing Framework represents a departure from the traditional focus on sickness absence reduction towards a more holistic, preventative approach. This evolution resonates deeply with my understanding that presenteeism, which relates to where staff attend work whilst unwell, often proves more detrimental to organisational performance than measured absence.
What strikes me most profoundly is the recognition that wellbeing cannot be treated as an isolated human resources function. Instead, it must be woven into the fabric of organisational culture, influenced by management capabilities, job quality, and social relationships at work. The framework’s seven domains provide a comprehensive lens through which to view organisational health, including small organisations like general practice, moving beyond simplistic interventions towards systemic cultural change.
A stark statistics underscore the urgency of this transformation. Mental health conditions remain the primary driver of sickness absence, with stress, depression, and anxiety accounting for 44% of all work-related ill health cases. Perhaps most troubling is the estimated £2.3 billion annual cost of bullying and harassment within the NHS, with 28.5% of staff reporting such experiences. These figures are not merely data points; they represent human suffering and organisational dysfunction that demand strategic intervention.

The Person-Centred Imperative for Workforce Wellbeing
Shifting from Systems to People
Person-Centred Intelligence (PCI) represents another critical evolution in how we conceptualise organisational health. The fundamental principle is that data should focus on people’s needs rather than system requirements. It challenges traditional performance management approaches. This shift from “what’s the matter with someone” to “what matters to someone” may appear subtle, yet it fundamentally reorients organisational priorities.
The evidence supporting person-centred approaches is compelling across multiple dimensions. Populations engaged in defining their own health outcomes demonstrate improved health behaviours and better results. Patients participating in care decisions report higher satisfaction, whilst collaborative health management reduces emergency service utilisation. Critically, increased patient engagement correlates with enhanced staff performance and morale, which creates a virtuous cycle that benefits all stakeholders.
Person-Reported Measures (PRMs) provide the mechanism for implementing PCI, capturing outcome, experience, and capability data directly from those affected. However, implementation requires careful consideration of purpose, population, and validated measurement tools. The ultimate test lies not in data collection but in how findings inform decisions and drive practice change.
Reflecting on my organisational context, I recognise that we often measure what is convenient rather than what matters. System-generated surveys are predominantly used, whilst the lived experiences of staff and patients remain under-represented. Adopting a person-centred approach would require uncomfortable conversations about whose perspectives we privilege and what outcomes we truly value.
Team Climate: The Critical Buffer
Understanding Relational Dynamics in your workforce
The evidence on team climate provides perhaps the most actionable insights for immediate practice. Whilst understaffing and workload pressures inevitably affect staff wellbeing and care quality, relational climate can serve as a crucial protective factor. Good team dynamics, stable structures, and participatory decision-making mitigate emotional exhaustion and maintain care quality even under demanding conditions.
This approach challenges the assumption that wellbeing primarily requires additional resources. Whilst adequate staffing remains essential, the quality of team relationships and the nature of the working climate significantly influence how teams experience and respond to pressure. A cohesive team with strong relational bonds and shared decision-making processes can sustain performance and wellbeing that poorly functioning teams cannot achieve, regardless of resource levels.

Good team climate is cultivated, not assembled. It requires ongoing attention to how the team functions together through fair leadership practices, conflict resolution, communication patterns, shared experiences, and organisational support. You could have a team of individually average performers with excellent climate, or a team of stars with terrible climate. The climate comes from the system and relationships, not the roster.
Team climate is built through consistent leadership behaviours over time, lived experiences that either build or erode trust, informal norms that develop organically, and day-to-day interactions that policies can’t script.
The Human Balance Sheet for Workforce Wellbeing
The application of NHS health and wellbeing framework suggests taking a data-first approach when exploring wellbeing, but I have struggled to find a helpful way of collecting staff wellbeing metrics that will be really transformational. Often, one source of data is not enough for an organisation to diagnose the root cause of the problem and multiple sources are needed to enable an organisation to make an informed decision on interventions.
Sickness absence alone is not enough. I feel that sourcing information from the NHS Survey metric can be tedious, and I anticipate most staff and leaders/managers would not find it applicable at a personal level, especially for small organisations like general practice.
To bridge this gap, I’ve created a conceptual framework for evaluating the strategic health and well-being of general practice staff (practitioner wellbeing) by applying principles from financial accounting.
This approach aims to create a “human balance sheet” to bring the same analytical rigour and intentionality to professional wellbeing that is typically applied to financial assets and liabilities.
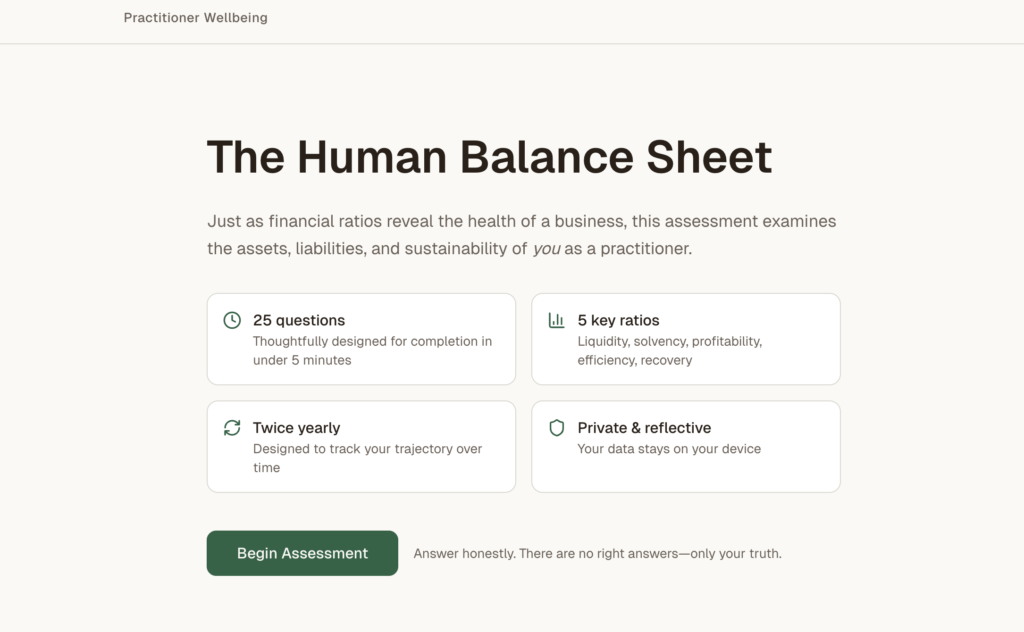
This framework challenged me to think differently about professional sustainability, treating wellbeing not as an abstract concept but as a measurable asset that can be systematically assessed and managed.
The distinction between human assets and liabilities provides a powerful analytical tool. Energy and vitality function as liquid assets, which are readily available resources for meeting immediate demands. Skills and competencies represent our professional capital, whilst relationships and trust serve as goodwill assets that facilitate collaborative work. Purpose and meaning, though intangible, emerge as the driving force behind sustained professional engagement.
Conversely, chronic stress and exhaustion operate as loans against our future selves; you can call them debts that accumulate interest in the form of deteriorating health and diminished performance. Unprocessed trauma, resentment, and cynicism erode our professional foundation, whilst skills erosion represents the depreciation of our human capital.
The measurement ratios offer particular insight. The Current Energy Ratio (Available Energy / Immediate Demands) and Debt-to-Energy Equity Ratio (Accumulated Stress / Core Vitality) provide objective indicators of professional sustainability. When the Interest Coverage Ratio (Joy & Fulfilment / Emotional Labour) falls below 1.0, we are operating at an emotional loss, a situation that cannot be sustained long-term.
This framework has profound implications for my own leadership practice. It suggests that workforce sustainability requires the same analytical discipline we apply to financial management. We must regularly audit human capital, identify opportunities for improvement, and make strategic interventions to restore balance. The question becomes: are we investing in our people’s assets, or simply depleting them until bankruptcy?
Here’s how you can help:
- Take the 5-minute assessment: https://v0-human-asset-analysis.vercel.app/
- Review your results (liquidity, solvency, profitability, efficiency, recovery ratios)
- Share honest feedback in the comments: Does the financial metaphor help or hinder? Is it relevant to your organisational setting? Would you actually use this twice a year? Does it capture what matters to you?
When you participate, you help validate a tool that spots depletion before crisis by giving you data to advocate for yourself and catch warning signs early. But if we don’t measure what matters, we’ll lose more practitioners to preventable burnout while surveys continue asking the wrong questions. Can you take 5 minutes to help test this? Thank you for your participation.
Read more about the practitioner wellbeing metrics we introduced earlier here.
Let’s Bring it All Together
Organising and synthesising these perspectives reveals a coherent strategic approach to organisational health. The NHS wellbeing framework provides the structural architecture, person-centred intelligence ensures we focus on what matters, team climate research identifies the critical relational mechanisms that mediate outcomes, and the human balance sheet offers measurement discipline.
The convergence is clear: sustainable healthcare organisations require proactive, systemic cultural change informed by measurable human data, delivered through person-centred approaches, and enacted within supportive team environments. This is not a linear process but an iterative cycle of assessment, intervention, and refinement.
Pros of using the Human Balance Sheet
For my leadership practice, this integrated framework suggests several priorities:
Person-Centred Design: Redesigning data collection and decision-making processes to genuinely privilege the perspectives of staff and patients.
Cultural Investment: Prioritising team climate and relational quality as strategic organisational resources, not merely desirable attributes.
Strategic Measurement: Implementing human capital audits alongside traditional performance metrics, ensuring we monitor staff wellbeing systematically, hence shifting from reactive crisis management to proactive wellbeing investment.
This exploration has fundamentally challenged my assumptions about organisational health management. I previously viewed wellbeing initiatives as separate from core operational strategy, important but peripheral. By producing and utilising the human-balance-sheet from the practitioner wellbeing survey. I now recognise that workforce wellbeing is the foundational mechanism for achieving all other organisational objectives. Without healthy, engaged, sustainable staff, no healthcare organisation can deliver quality care or maintain financial viability.
The financial metaphor of the human balance sheet particularly resonates because it speaks the language of organisational decision-makers. By framing wellbeing in terms of assets, liabilities, solvency, and return on investment, we can elevate workforce health from a human resources concern to a strategic imperative that commands boardroom attention and resource allocation.
Cons of using the Human Balance Sheet
However, I also recognise the limitations and challenges of this metric.
The Human Balance Sheet can be a helpful starting point as long as it’s used to inform deeper conversations, not replace them. It shouldn’t be the only measure of wellbeing, nor should it be used in isolation from qualitative feedback, team dialogue, and structural improvements (e.g., workload, support systems, leadership training).
Person-centred approaches require genuine power-sharing that may threaten existing hierarchies. When you genuinely share power with employees (letting them have real say in decisions, work design, and resource allocation), this could directly challenge the authority and control that managers and senior leaders currently hold. The key safeguard is ensuring power-sharing comes with clear boundaries, transparency, and genuine accountability mechanisms for all parties.
Team climate interventions require sustained cultural change that cannot be achieved solely through policy.
Conclusion and Future Direction
The evidence is unequivocal: optimising the human component, our staff, is essential for improving patient outcomes and organisational sustainability. This requires moving beyond rhetoric to implement systematic, measured, person-centred approaches that prioritise relational quality and team climate.
As a leader operating within this complex environment, my challenge is to translate these insights into tangible practice. This means advocating for human capital audits, investing in team development, redesigning measurement systems, and modelling the cultural values we espouse. It means having difficult conversations about resource allocation, acknowledging that short-term productivity gains may often represent long-term human capital depletion.
Most importantly, it requires recognising that organisational health is not a destination but a continuous journey of assessment, learning, and adaptation. The frameworks and evidence presented here provide a roadmap, but each organisation must navigate its own path, informed by its unique context, challenges, and aspirations.
In closing, one question will guide my ongoing practice: are we actively building human capacity, or quietly depleting it? How we answer this will determine not only workforce wellbeing, but the future sustainability of our healthcare system.
References
Dale, J., Potter, R., Owen, K., Parsons, N., Realpe, A. and Leach, J. (2015) ‘Retaining the General Practitioner Workforce in England: What Matters to GPs? A Cross-sectional Study’, BMC Family Practice, 16(1), pp. 1-10.
Doran, N., Fox, F., Rodham, K., Taylor, G. and Harris, M. (2016) ‘Lost to the NHS: A Mixed Methods Study of Why GPs Leave Practice Early in England’, British Journal of General Practice, 66(643), pp. e128-e135.
Panagioti, M., Geraghty, K., Johnson, J., Zhou, A., Panagopoulou, E., Chew-Graham, C., Peters, D., Hodkinson, A., Riley, R. and Esmail, A. (2018) ‘Association Between Physician Burnout and Patient Safety, Professionalism, and Patient Satisfaction: A Systematic Review and Meta-analysis’, JAMA Internal Medicine, 178(10), pp. 1317-1331.
West, M.A., Lyubovnikova, J., Eckert, R. and Denis, J.L. (2014) ‘Collective Leadership for Cultures of High Quality Health Care’, Journal of Organizational Effectiveness: People and Performance, 1(3), pp. 240-260.
Scheepers, R.A., Boerebach, B.C.M., Arah, O.A., Heineman, M.J. and Lombarts, K.M.J.M.H. (2015). A Systematic Review of the Impact of Physicians’ Occupational Well-Being on the Quality of Patient Care. International Journal of Behavioral Medicine, [online] 22(6), pp.683–698. doi:https://doi.org/10.1007/s12529-015-9473-3.
https://www.hse.gov.uk/statistics/assets/docs/stress.pdf
https://www.researchgate.net/publication/228873678_Human_Capital_and_the_Balance_Sheet



