One of the core aspects of GP consultation techniques is using the ICE Impact framework to achieve a joint management plan. For those who aren’t familiar, this involves the GP facilitating the consultation in a way that elicits the patient’s agenda and applies critical reasoning and good communication skills to create a collaborative management plan.
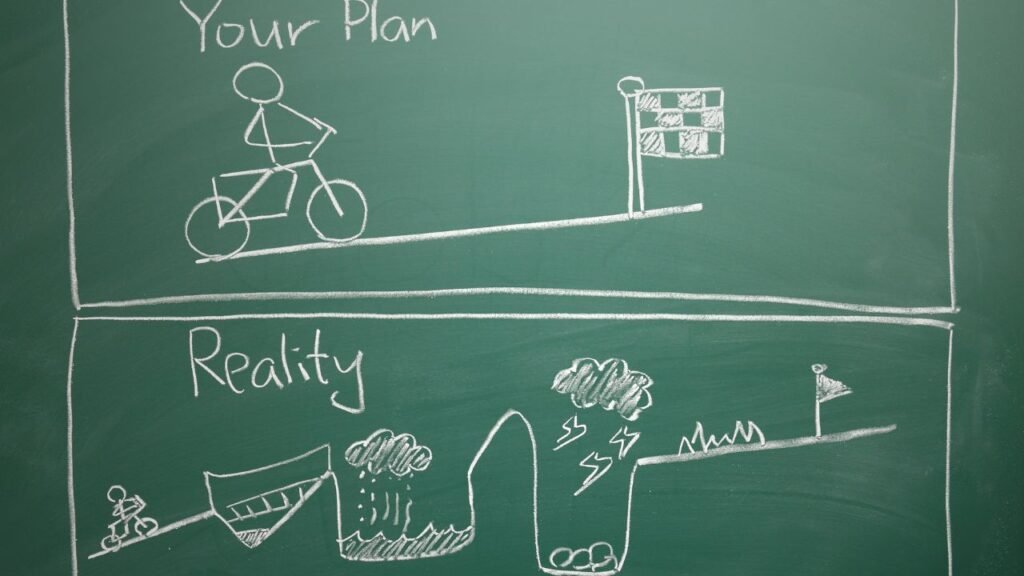
In reality, it’s not always as smooth as it sounds. Sometimes steps could be missed, an occasional backtrack to gather more information, or the repetition of already said facts.
These patient interactions make up the bulk of a primary care clinician’s day. A GP might see about 30 patients daily, not including other tasks and administrative duties that involve contacting patients directly outside scheduled appointments. Doing this 4-5 days a week, year after year, can be quite challenging.
One of the most challenging pitfalls is when a clinician fails to acknowledge the reality a patient is trying to convey during a consultation. This can lead to a mismatch in the management plan, causing distress for both patients and clinicians. Other examples of difficult consultations involves conversations around opioid dependence, drug use, functional illness, chronic mental health illness or clear uncertainty.
Furthermore, communication among staff especially if they feel unsupported in the organisation are equally sources of distress that can lead to burnout. Read more here.
It’s not immediately clear how many distressing consultations it takes for a clinician to start feeling overwhelmed. While most consultations go smoothly and are mutually beneficial, those difficult ones can be hard to handle.
When addressing burnout., it’s important to reflect on distressing consultations as either a root cause or a symptom of burnout. If it’s a root cause, seeking out coaching from a mentor or colleague can be helpful. If it’s a symptom of burnout, it’s crucial to recognise when you’re no longer mindfully aware of situations and yourself.
So, how do you manage distress to prevent burnout?
Primary care clinicians generally show great tolerance. When faced with a difficult situation or consultation, you need the resilience to endure the emotional toll, especially when you’re tired, like during the afternoon session.
In light of this, practices that schedule a higher number of patient contacts in the morning and a little less in the afternoon might find this setup beneficial. This system allows you to use your morning energy for most of the day’s decisions and may reduce burnout.
When a consultation isn’t going well, one way to cope is to practice radical acceptance. Acceptance means being willing to experience the situation as it is, rather than how we want it to be. When the clinician’s agenda is imposed on the patient’s story, it can lead to difficult conversations.

Radical acceptance is a mindfulness concept from Dialectical Behavior Therapy (DBT) that helps individuals acknowledge difficult situations without unnecessary emotional distress. Importantly, it does not mean judging a negative situation as good, nor does it mean giving permission for the situation to persist indefinitely. It’s about recognising the current reality without attaching judgments of good or bad. Additionally, radical acceptance does not imply giving up your options or feeling powerless. Instead, it involves accepting the present moment fully while maintaining the agency to explore and pursue changes or improvements. This approach helps in reducing emotional suffering and leads to a more constructive engagement with the situation at hand.
It can be an adventure to accept a patient’s story as it is, rather than imposing one’s own will on the consultation. By letting the history and examination guide the conversation and allowing the patient to make a joint decision can lead better professional relationships, which is not only rewarding in itself but essential for long-term practice in primary care.
When clinicians show genuine empathy and understanding, patients are more likely to feel valued and heard, leading to better communication and cooperation.
It takes incredible honesty and skill to describe things as you see them, especially when there’s a mismatch in agenda.
Radical acceptance involves fully acknowledging and accepting a patient’s situation without judgment or emotional resistance. By embracing radical acceptance, you can remain present and empathetic with your patients, which can lead to genuine connections that reduce your own emotional distress and reinforce your commitment to your profession.
Overall, maintaining mindful awareness of where you are in the consultation and your overall mood throughout the day can be a valuable resource for tolerating distress and maintaining your well-being.
Best wishes in your career.
References
Hall, L.H., Johnson, J., Watt, I. and O’Connor, D.B. (2019). Association of GP wellbeing and burnout with patient safety in UK primary care: a cross-sectional survey. British Journal of General Practice, 69(684), pp.e507–e514. doi:https://doi.org/10.3399/bjgp19x702713.